Introduction
Molecular MRD assays targeting NPM1 mutant (mut) transcripts have an established role for monitoring treatment efficacy in patients with NPM1mut AML. Approximately 25% of NPM1mut patients show persistent MRD level in the bone marrow (BM) at the end of treatment (EOT), which is associated with a higher risk of relapse (Ivey, NEJM 2016; Kronke, JCO 2011). Molecular persistence at low copy number (MP-LCN) is defined by the European LeukemiaNet (ELN) as MRD positivity in patients in morphological complete remission (CR) with <1000-2000 transcripts per 105ABL and a relative increase of <1 log between any two positive samples collected after EOT (Schuurhuis, Blood 2018). The UK NCRI working group recently reported the impact of NPM1mut MRD burden and FLT3-ITD status on risk of relapse after allogeneic stem cell transplantation (Dillon, Blood 2020), however the clinical relevance of NPM1mut MP-LCN in patients who are not transplanted is unknown. We aimed to characterize the natural history of persistent NPM1mut MRD after chemotherapy and to identify factors associated with subsequent disease progression.
Methods
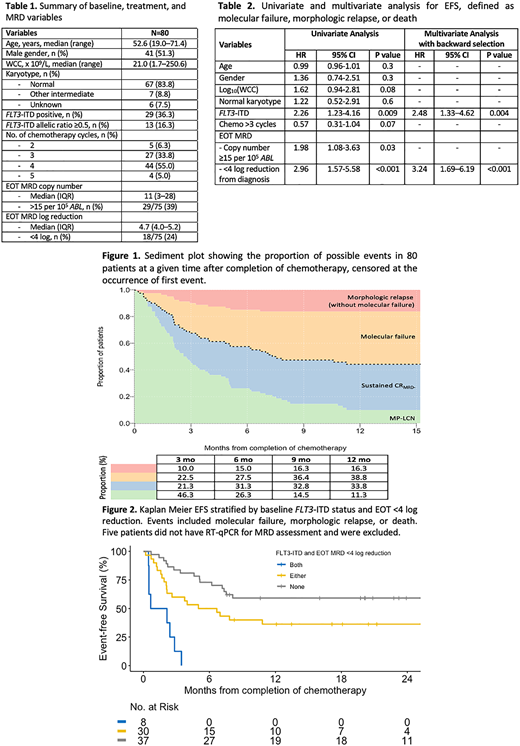
Consecutive patients with newly diagnosed NPM1mut AML receiving at least 2 cycles of intensive chemotherapy were included if MRD remained detectable at EOT. UK patients were all enrolled in the NCRI AML17 and AML19 studies. Australian patients were retrospectively identified. BM samples were analyzed by either RT-qPCR (n=75) (Ivey, NEJM 2016) or ultra-deep next-generation sequencing (UD-NGS, n=5, excluded from Cox model). We applied the ELN definitions for molecular progression or relapse (considered together as molecular failure [MF]), MP-LCN and complete molecular remission (CRMRD-). Kaplan Meier survival estimates were calculated from EOT to death (OS), and/or morphologic relapse (RFS), and/or MF (EFS). The optimal NPM1mut expression threshold was pre-determined by recursive partitioning. Variables with p<0.1 from univariate analysis were included in the final multivariate Cox model and confirmed by backward selection method. Copy numbers are expressed per 105ABL copies (for RT-qPCR) or as percentage of total reads (for UD-NGS).
Results
A total of 80 patients had NPM1mut detectable at a median of 37 days (range 19-90; 12 [15%] were >60 days) from last course of chemotherapy; characteristics summarized in Table 1. The majority of patients (89%) had received 3-4 cycles of chemotherapy. At EOT, the median NPM1mut transcript level by RT-qPCR was 11 copies (range 0.3-8699; 3 were >2000) and median reduction from baseline was 4.7 log (range 2.1-6.0). A total of 34 patients (45%; 4 not monitored) fulfilled the criteria for MP-LCN.
With a median follow-up time of 24 mo (range 8-77), 27 (34%) spontaneously achieved a sustained CRMRD- for >6 months, 31 (39%) had MF and 13 (16%) had morphologic relapse without preceding MF (due to rapid relapse [n=8], lack of monitoring [n=3], extramedullary or NPM1 wild-type relapse [n=1 each]) (Figure 1). Nine patients (11%) had persisting MP-LCN (included transient MRD negativity): median interval between EOT to the last known positive sample was 12 mo (range 3-32), and all patients currently remain alive and without morphologic relapse by the data cut-off date July 13, 2020.
Next, we examined the variables associated with MF and/or morphologic relapse. In univariate analysis, factors associated (p<0.1) with disease progression were white cell count, FLT3-ITD, <4 cycles of chemotherapy received, EOT NPM1mut ≥15 copies, and <4 log reduction from baseline (Table 2). In multivariate analysis (and confirmed by backward selection), only baseline FLT3-ITD (HR 2.5, 95% CI 1.3-4.6) and EOT NPM1mut MRD <4 log reduction from baseline (HR 3.2, 95% CI 1.7-6.2) retained significance. Patients with none, either, or both of these features had a median EFS of not reached, 5.8 and 1.4 mo, respectively (Figure 2). The corresponding 2-year RFS was 73%, 54% and 0% (median 3.5 mo).
Conclusions
We describe the natural history of patients with NPM1 mutated AML who remain MRD positive after completing intensive chemotherapy. Almost half either spontaneously achieve MRD-negativity or have stable low-level expression without relapse with minimum follow up of 8 mo. Patients with both FLT3-ITD and <4 log reduction in transcript levels at the end of therapy are at very high risk of disease progression and warrant consideration of pre-emptive treatment.
Tiong:Pfizer: Consultancy; Servier: Consultancy; Amgen: Consultancy, Honoraria. Dillon:Abbvie: Honoraria, Research Funding; Novartis: Honoraria; Menarini: Honoraria; Astellas: Honoraria; Pfizer: Honoraria, Research Funding; Jazz Pharmaceuticals: Honoraria; Amgen: Honoraria, Research Funding. Bajel:Abbvie: Honoraria; Pfizer: Honoraria; Amgen: Honoraria, Speakers Bureau; Novartis: Honoraria; Astellas: Honoraria. Russell:Pfizer: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Speakers Bureau; Astellas: Membership on an entity's Board of Directors or advisory committees; Jazz: Research Funding, Speakers Bureau. Wei:MacroGenics: Consultancy, Honoraria; Pfizer: Honoraria; Servier: Consultancy, Honoraria, Research Funding; Walter and Eliza Hall Institute: Other: former employee and receives a fraction of its royalty stream related to venetoclax; Celgene: Consultancy, Honoraria, Research Funding; AbbVie Inc.: Consultancy, Honoraria, Research Funding; Genentech: Honoraria; Astra Zeneca: Honoraria, Research Funding; Janssen: Consultancy, Honoraria; Astellas: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal